Nutrition
Objective
Under POSHAN Abhiyaan, achieve the following outcomes by 2022-23, compared to the baseline of 2015-16 (National Family Health Survey-4):
Reduce the prevalence of stunting among children to 25 per cent or less.
Reduce the prevalence of underweight in children (0-6 years) to 25 per cent or less.
Reduce the prevalence of anaemia among young children (6-59 months) to 43 per cent or less.
Reduce the prevalence of anaemia among adolescent girls and women (15-49 years) to 38 per cent or less.
Current Situation
Under-nutrition is the prime risk factor in over 40 per cent of under-five child deaths. Children with under-nutrition, anaemia and iodine deficiency will have low IQ scores and productivity as adults. A World Bank estimate1 indicates that reducing stunting can raise India’s GDP by 4-11 per cent. The prevalence of stunting declines by an estimated 3.2 per cent for every 10 per cent increase in income per capita. Similarly, a 10 per cent rise in income per capita translates into a 7.4 per cent fall in wasting. Thus, increasing per capita incomes through rapid and equitable economic growth is a necessary condition for improving nutrition outcomes.
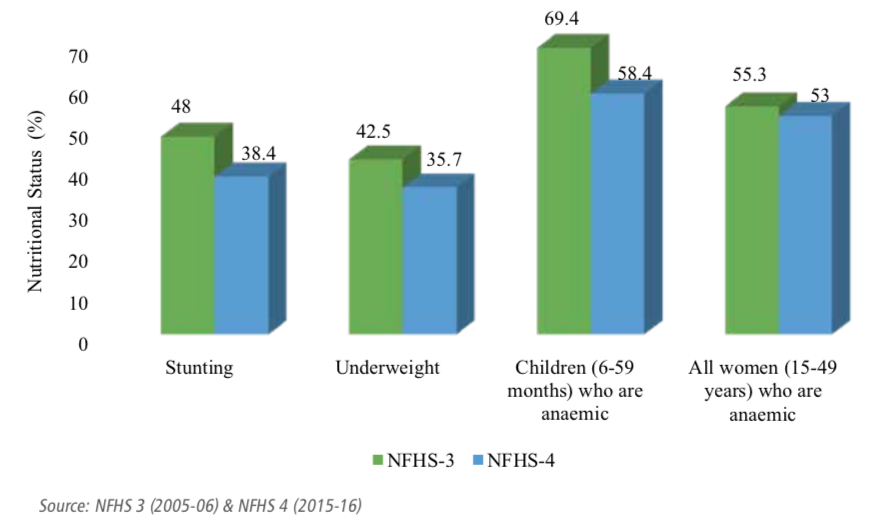
Figure 31.1: Key nutritional indicators in India
 Note: Image taken from Niti Aayog - Strategy for New India@75 Document
Note: Image taken from Niti Aayog - Strategy for New India@75 Document
Although progress has been made, according to National Family Health Survey-4 (NFHS-4), 2015-16, over one-third of all under-five children are stunted (low height-for-age), every fifth child is wasted (low weight-for-height), and more than 50 per cent of the children are anaemic.
Other emerging economies such as Brazil (stunting – 6.1 per cent, wasting – 1.6 per cent), China (stunting – 6.8 per cent, wasting – 2.1 per cent) and Mexico (stunting – 13.6 per cent, wasting – 1.6 per cent) fare far better on nutrition indicators compared to India.
Ironically, at the same time, India is also grappling with the rising menace of ‘over-nutrition’. Nearly one fifth of India’s adults are either obese or overweight as per NFHS-4 data, leading to an increased risk of diabetes and cardiovascular disorders.
India can leverage its demographic dividend only if its citizens attain optimum levels of health, nutrition and cognition. Recognising this, the government launched the POSHAN Abhiyaan in March, 2018 to provide police and programmatic guidance to high burden states and districts, facilitate multisectoral planning, catalyse resource mobilisation and develop a surveillance system for nutrition.
Constraints
1. Multidimensional determinants of under- nutrition are inadequately reflected in policymaking
Inadequate and poor-quality food is an important, but not the only, cause of under-nutrition.
The underlying causes of malnutrition are multifaceted and rooted in economic and social factors like low levels of female literacy, lack of access to clean drinking water and sanitation.
At a more proximate level, nearly half of childhood under-nutrition is attributable to illnesses (in particular, diarrhoea, pneumonia and measles) and foetal growth restriction that results in low birth weight due to maternal nutrition, maternal health, pregnancy complications and epigenetic factors.
2. Design limitations of the Integrated Child Development Services (ICDS)
- The design of the ICDS programme has an important limitation – its focus on the first 1000 days of the child’s life is inadequate. Over 80 per cent of brain growth occurs during the first 1000 days of a child’s life. This has a significant bearing on work capacity, productivity and IQ in adulthood. Hence, nutrition programmes in the country must accord the highest priority to this critical period of life. However, the ICDS programme’s most prominent activities are focused on the delivery of pre-school education and hot cooked meals as well as growth monitoring at anganwadi centres for children between 3 and 6 years. Only 10% of children between 6 and 13 months received an adequate diet in 2015-16 (NFHS-4).
3. ICDS programme implementation
The ICDS programme is beset with persistent challenges such as shortage of staff and field workers, poor monitoring, instances of food pilferage and poor quality of services.
Given the complex nature of the challenge, a multi-dimensional approach is a must. NITI Aayog has already detailed a possible action agenda in its National Nutrition Strategy, which needs to be urgently implemented.
Way Forward
1. Address policy and governance issues
Context-specific Implementation
Provide greater flexibility to states under the
POSHAN Abhiyaanto adapt programmes for context-specific implementation and to experiment with innovative approaches to attain high coverage, quality, equity and better outcomes.Establish an institutional mechanism, outside the government, to conduct independent annual audits of the programme to achieve implementation improvements.
2. Ensure convergent action at all levels
Integrated Health, Nutrition and Swachh Bharat Mission (SBM)
Develop and implement Annual Integrated Health, Nutrition and Swachh Bharat Mission (SBM) action plans for all districts under the POSHAN Abhiyaan.
Ensure accountability of the local administration.
Actively engage panchayati raj institutions, the public distribution system (PDS) and public health engineering departments for delivery of the action plans.
Integrate health, SBM and nutrition services at the village level through the Village Health, Sanitation and Nutrition Committees and by ensuring regular observance of Village Health Sanitation and Nutrition Days (VHSNDs).
Develop an implementation guide for integrated action for nutrition (‘a cook book’) for district administrators.
Establish a state-level convergence mechanism for nutrition under the chief secretary/ equivalent officer and corresponding structures at the district and block levels.
3. Implement mission mode action in districts with a high burden of malnutrition under POSHAN Abhiyaan
State, District and Block Levels Implementation
- Set up convergence mechanisms at the state, district and block levels; develop action plans specifying timelines; ensure sufficient budgetary allocation; strengthen monitoring systems; galvanize coordination; demonstrate change guided by annual surveys and intensively monitor implementation by NITI Aayog
4. Refine programme interventions
Focus on first 1000 days
As envisaged under the POSHAN Abhiyaan, devise a strategy for additional home-based contacts under the home-based young child care initiative with:
Mothers having children in the age group of 3 months to 2 years to ensure compliance with infant and young child feeding practices as well as healthy behaviours.
Mothers having a child with moderate or severe malnutrition for regular follow-up.
These home visits should be conducted by accredited social health activists, a second auxiliary nurse midwife or community infant and young child feeding counsellors.
Replace the food-centric approach with more broad-based action that includes healthcare measures (special care of low birth weight in- fants and immunization), birth spacing, delaying age of marriage, exclusive breastfeeding for 6 months, and timely and adequate access to complementary food interventions.
Focus on immunization including Rota Virus and Pneumococcal Vaccines; target the vaccines preferentially to high focus districts.
Fortification
Consider mandatory fortification of staples produced in the organized sector and provide incentives to the industry to do so.
Incorporate fortified food grains and double fortified salt within government programmes such as ICDS, mid-day meal scheme, and PDS.
Explore approaches to bio-fortification of grains for micronutrient deficiencies.
Research
- Create a national nutrition surveillance system to track food quality and consumption patterns and nutritional deficiency profiles for all age groups in different regions.
• Conduct implementation research studies to inform improvements in the programme.
Key research areas include assessing the effectiveness of conditional cash transfers/ vouchers in improving child nutrition and the optimum formulation of supplementary nutrition for young children.
Evaluate ICDS programme in depth and suggest reforms for greater effectiveness.
Track changes in birth weight and prematurity rates at the population level; conduct long-term cohort studies on changes in body composition and early biomarkers of metabolic disorders.
Review and redesign nutrition programmes targeted at adolescent girls; link these with pre-pregnancy interventions.
Test approaches to prevent childhood and adult obesity at the population level.
5. Scale-up nutrition MIS and strengthen monitoring mechanisms
IT-based real time monitoring
Establish an
IT-based real time monitoring mechanismby rolling out the Common Application Software (CAS) developed by the Ministry of Women and Child Development on a countrywide basis.Undertake joint health and nutrition reviews in the field as a standard practice.
Establish accountability with defined responsibilities at all levels – state, district and field.
6. Make ‘POSHAN Abhiyaan’ a Jan Andolan
Community-led Movement
Make POSHAN Abhiyaan a community-led movement with adequate political backing.
Develop behavioural change communication modules and ensure its use by all frontline workers, especially during VHSNDs; emphasise individual as well as group counselling.
7. Galvanize the National Anaemia Control Programme
Anaemia Control Programme
Implement the revised strategy for the anaemia control programme based on evidence; incorporate home, community, school and facility level action; embed the strategy in the activities of the emerging health and wellness centres.
Consider ‘screen and treat’ as a part of the anaemia control intervention package.