Public Health Magement and Action
Objective
To revamp radically the public and preventive health system in the nation through the following strategic interventions:
Mobilize public health action through an integrated, inter-sectoral and pan-stakeholder approach, targeted at communities and individuals as well as grassroots organizations, aimed at creating an unprecedented people-led movement for health and wellness.
Operationalize vital enablers - (a) public health and management cadre, (b) public health agency with capacitated supporting institutions (c) municipalities and panchayati raj institutions.
Current Situation
Public health, i.e., the science of keeping communities healthy through the prevention of disease and promotion of health and wellness, has historically been a low priority in India. Of the total current expenditure on health classified by healthcare functions, preventive care accounts for 6.7 per cent. The money spent on curing people on the other hand is 51 per cent of the expenditure1 with the remaining money being spent on pharmaceuticals, other medical goods and patient transportation.
Although India accounted for only 18 per cent of the global population in 2016, we accounted for 34 per cent of the global tuberculosis burden and 26 per cent of the premature mortality due to diarrhoea, lower respiratory and other common infectious diseases. At the same time, non-communicable diseases (NCDs), including cardiovascular conditions, chronic obstructive respiratory diseases, diabetes, mental health conditions and cancers are now the leading cause of health loss, with 55 per cent morbidity and premature mortality attributable to these conditions. The range of health loss3 across states is wide. Kerala and Goa have the lowest rates while Assam, Uttar Pradesh and Chhattisgarh have the highest rates.
Public health action and management is a scientific and professional endeavour which should not be left to untrained employees relying on common sense alone.
A suboptimal public health system:
Makes it challenging to tackle NCDs, which, in the first place, is all about prevention and early detection.
Causes us to resort to high-cost secondary and tertiary health care in many cases.
Diminishes our preparedness for new and emerging threats such as bioterrorism.
Compromises our ability to harness the demographic dividend.
The nations with whom we compete or aspire to emulate have achieved health and wellness outcomes on the foundation of strong public health systems. Thus, it is an absolutely essential ingredient for building a New India.
During the last four years, the government has taken several steps to strengthen public health in the country including the launch of Mission Indradhanush and Intensified Mission Indradhanush as well as the National AYUSH Mission. Efforts have also been intensified for eliminating Neglected Tropical Diseases like Kala Azar and Lymphatic Filariasis. Further, the war against Tuberculosis has been escalated through the launch of the National Strategic Plan in 2017.
Constraints
Diseases need to be prevented first, a concept that has historically been inadequately acknowledged in India. The large burden of NCDs requires lifestyle and community-level interventions. Ensuring people eat right, sleep right, maintain good hygiene, exercise, and adopt a healthy lifestyle necessitates concerted interventions at various levels of the system.
In most states, population health management positions are staffed by doctors, trained primarily in the provision of curative services, or by generalist civil servants. They have limited public health training, which includes an understanding of the causes and linkages between risk factors and diseases as well as disciplines including epidemiology, biostatistics, social and behavioural sciences and management of health services. Likewise, hospitals are run by clinicians with little expertise in managing health facilities.
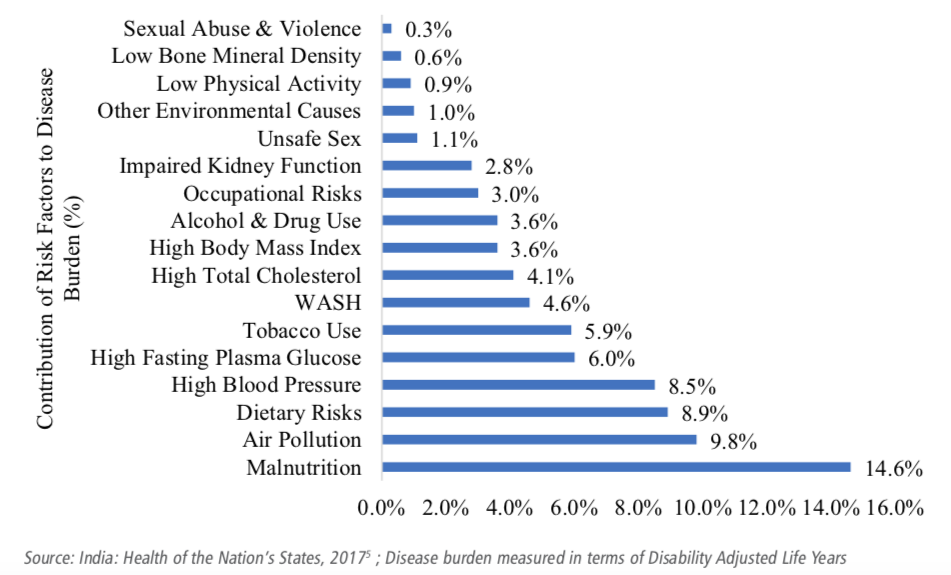
Figure 27.1: Preventable risk factors are the biggest contributors to the disease burden, 2016
 Note: Image taken from Niti Aayog - Strategy for New India@75 Document
Note: Image taken from Niti Aayog - Strategy for New India@75 Document
The following preventable risk factors are causes for a major proportion of diseases in the country: maternal and child malnutrition, air pollution, unhealthy diets, high blood pressure, high blood glucose, tobacco consumption, unsafe water, and poor sanitary practices; of these, nutrition, environment, water and sanitation are outside the purview of the health ministry. Therefore, accountability for ensuring vital public health actions is spread thin.
There is no single authority responsible for public health that is legally empowered to enforce compliance from other public authorities and citizens, even though several factors may require inter-sectoral action to achieve a measurable impact on population health.
Way Forward
1. Mobilize public health action at multiple levels
Appropriate Policy Measures
Public funding on health should be increased to at least 2.5 per cent of GDP as envisaged in the National Health Policy, 2017.
Create an environment, through appropriate policy measures, that encourages healthy choices and behaviours:
Make the practice of yoga a regular activity in all schools through certified instructors.
Increase taxes on tobacco, alcohol and unhealthy foods such as soda and sugar sweetened beverages.
Co-locate AYUSH services in at least 50 per cent of primary health centres, 70 per cent of community health centres and 100 per cent of district hospitals by 2022-23
Strengthen the Village Health Sanitation and Nutrition Day platform to cover a broader set of health issues across various population groups instead of only focusing on child health.
Activate multiple channels (schools, colleges, women’s groups, traditional events like fairs, social media platforms, National Cadet Corps etc.) and prepare communication materials for catalysing behavioural change towards greater recognition of preventive health care.
Make nutrition, water and sanitation part of the core functions of
panchayati raj institutionsandmunicipalities.
2. Institute a public health and management cadre in states
Creating a Dedicated Cadre for Public Health
Incentivize state governments to invest in creating a dedicated cadre for public health at the state, district and block levels:
Characteristics of the cadre
Train officials in public health related disciplines including epidemiology, biostatistics, demography and social and behavioural sciences.
Provide training in hospital management to suitably equip personnel responsible for managing large facilities.
Create a career pathway up to the highest levels within the state health departments for those trained in public health, as well as for those with clinical specialties.
Allow mid-level providers responsible for managing health and wellness centres delivering comprehensive primary healthcare to rise to higher-level positions within the cadre. Similarly, allow public health functionaries at the block and district levels to enter the cadre.
Mandate a master’s level qualification, in addition to specified training, for officials taking on leadership positions.
Institutional mechanisms
Develop a model public health and management cadre by drawing upon best practices and engage with states to adapt, refine and institutionalize the model.
Formulate guidelines to create the cadre, primarily by re-aligning the requisite skill sets of existing functionaries with service conditions.
3. Create a focal point for public health at the central level with state counterparts
Create Autonomous Focal Agency
Create a designated and autonomous focal agency with the required capacities and linkages to perform the functions of disease surveillance, information gathering on the health impact of policies of key non-health departments, maintenance of national health statistics, enforcement of public health regulations, and dissemination of information to the public. An appropriately empowered and capacitated National Centre for Disease Control may be considered to play this role with support from relevant organizations.
Create a counterpart Public Health Agency in each state, where they do not already exist.
4. Miscellaneous
Need for a Public Health Act
Explore the need for a Public Health Act to legislatively empower and, if necessary, institutionalise the Public Health Agency discussed above.
Redefine the role of the technical directorate (Directorate General of Health Services) and create a Directorate of Public Health.
Develop a comprehensive MIS including baseline data for NCDs.